Indirect
opthalmoscopy with direct ophthalmoscope as light
source
Ai-Hou
Wang, M.D. Ph.D.
Pediatric
ophthalmological examinations often use direct ophthalmoscopes for Hirschberg
corneal light reflex strabismus test, interocular distance measurement during
spectacle fitting, and other procedures. Clinical experience has shown that
indirect ophthalmoscopy for fundus examination, including fundus torsion test,
will be more convenient if using a direct ophthalmoscope as the light source
(see figure).
How
many of you ophthalmologists have actually done this?


If you
look through the observing hole of a direct ophthalmoscope, corneal light reflex
would interfere with the fundus image. Therefore, we usually
view close to the upper edge of the ophthalmoscope. This is similar
to Neitz handheld indirect ophthalmoscope, where the visual line is
typically from its upper edge (see figure).




The
upper part of the light source of Neitz handheld indirect ophthalmoscope is
borderless, allowing for extremely close between the visual line and the light path.
This is crucial for indirect ophthalmoscopic fundus examination.
In
direct ophthalmoscopes, the light path is almost at the same level as the
viewing hole. There is a space between the instrument
border and the viewing hole. Among the direct ophthalmoscopes from four
well-known brands – Neitz (Japan), Welch Allyn (USA), Heine (Germany), and
Keeler (UK) (see figure) – Heine has a shortest of this space (d) (see figure).
This configuration makes it best suitable for indirect ophthalmoscopy, when the
visual line is from the upper edge of the instrument.

The
optics of indirect ophthalmoscopy – specifically, the distance between the visual
line and the light path – are similar to those of
photorefraction. If the distance is too short (as observing through the viewing
hole of direct ophthalmoscope), corneal light reflex will interfere; if it’s too
long (as viewing along the upper border of direct ophthalmoscope), the dark
zone of photorefraction will make the fundus invisible.
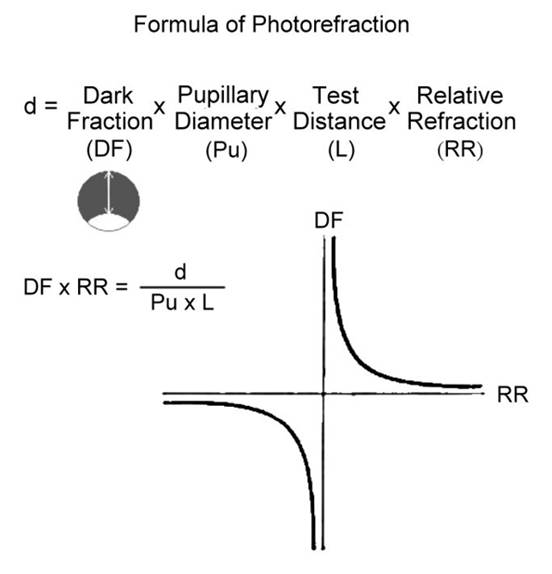
The
formula for photorefraction is shown in the figure, where d
is the distance between the visual line and the light path, and is the
product of (1) the ratio of the dark area to the pupil (Dark Fraction), (2) the
pupillary diameter, (3) the test distance, and (4) the relative refraction (see
figure).
Relative
refraction refers to the refraction with the reciprocal of the test distance as
the zero point. For example, at a test distance of 50cm, -2D (1/0.5m) is the
zero point. The relative refraction of -2D is 0D [(-2D)-(-2D)=0D], the relative refraction of -4D is -2D [(-4D)-(-2D)=-2D], and the relative
refraction of +1D is +3D [(+1D)-(-2D)=+3D].
With a
fixed d-value, fixed pupil size, and fixed testing distance, the relationship between
refraction and dark fraction exhibits a hyperbolic relationship (see figure).
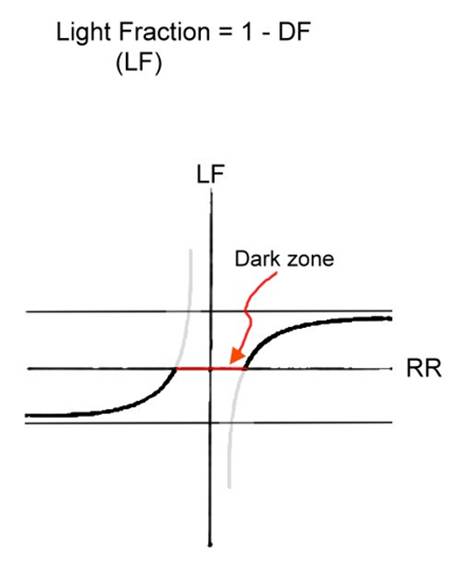
Many
photorefractive instruments measure the light fraction of the pupil, also known
as the crescent reflex. The light fraction is 1-dark fraction (DF). The
relationship between refraction and light fraction is thus shown on the figure
– the larger the refraction, the larger the light fraction (crescent). However,
in high refractive errors, the size of the light fraction reaches a plateau,
resulting in decreased resolution in reading the refractive value.
A
large d-value results in a relatively large dark zone in areas of low
refractive error (see figure), meaning that the red reflex of the pupil is not
visible over a relatively large range of low refractive errors (most people
have relatively low refractive errors). A small d-value results in a smaller
dark zone, where the red reflex of the pupil is not visible only in a
relatively small range of low refractive errors.
Returning
to the topic of ‘using direct ophthalmoscope as the light source of indirect
ophthalmoscopy, a larger d value will result in a larger dark zone. In most
people with lower refractive error, the red reflex of the pupil will be invisible and the fundus examination will thus be impossible.

If
direct ophthalmoscope manufacturers would make the edge above the viewing hole
as shorter as possible, or even make it as the Neitz
handheld indirect ophthalmoscope which has no upper edge, then direct and
indirect ophthalmoscopes could be combined into one, which would be really terrific!